RESEARCH
Our multidisciplinary team conducts translational “bench to bedside” research and collaborates with physicians and scientists locally, nationally, and internationally to advance scientific knowledge and clinical care in neurogenetics and neonatology.
PRECISION MEDICINE FOR NEONATAL AND INFANTILE EPILEPSIES
The highest incidence of epilepsy in childhood is in the first year of life, affecting 1 in 1000 infants. Infantile epilepsies are associated with morbidity, notably drug-resistant seizures and impaired developmental outcomes, and increased mortality. Although most infantile epilepsies are believed to have genetic causes, most infants with epilepsy remain genetically “unsolved,” which limits our ability to develop effective precision therapies and ultimately improve outcomes. We discover underlying genetic causes of infantile epilepsies using genomic and multiomic methods, evaluate the impact of these discoveries on infants with epilepsy and their families, including assessing amenability to emerging precision therapies, and identify strategies for equitable implementation of precision medicine for this population. Our collaborative Gene-STEPS study—the first study of rapid sequencing in a disease-specific cohort—demonstrated the feasibility, diagnostic yield, and clinical utility of rapid genome sequencing in infantile epilepsies.
Molecular genetic mechanisms of pediatric epilepsies
Epilepsy is the most common neurological disorder of childhood worldwide. We use exome sequencing, genome sequencing, long read sequencing, and additional genomic sequencing methods coupled with comprehensive bioinformatics analyses to discover molecular genetic mechanisms underlying pediatric epilepsies. We recently demonstrated the utility of genome sequencing after non-diagnostic exome sequencing for this population.
SOMATIC MOSAICISM IN EPILEPSY AND RELATED DISORDERS
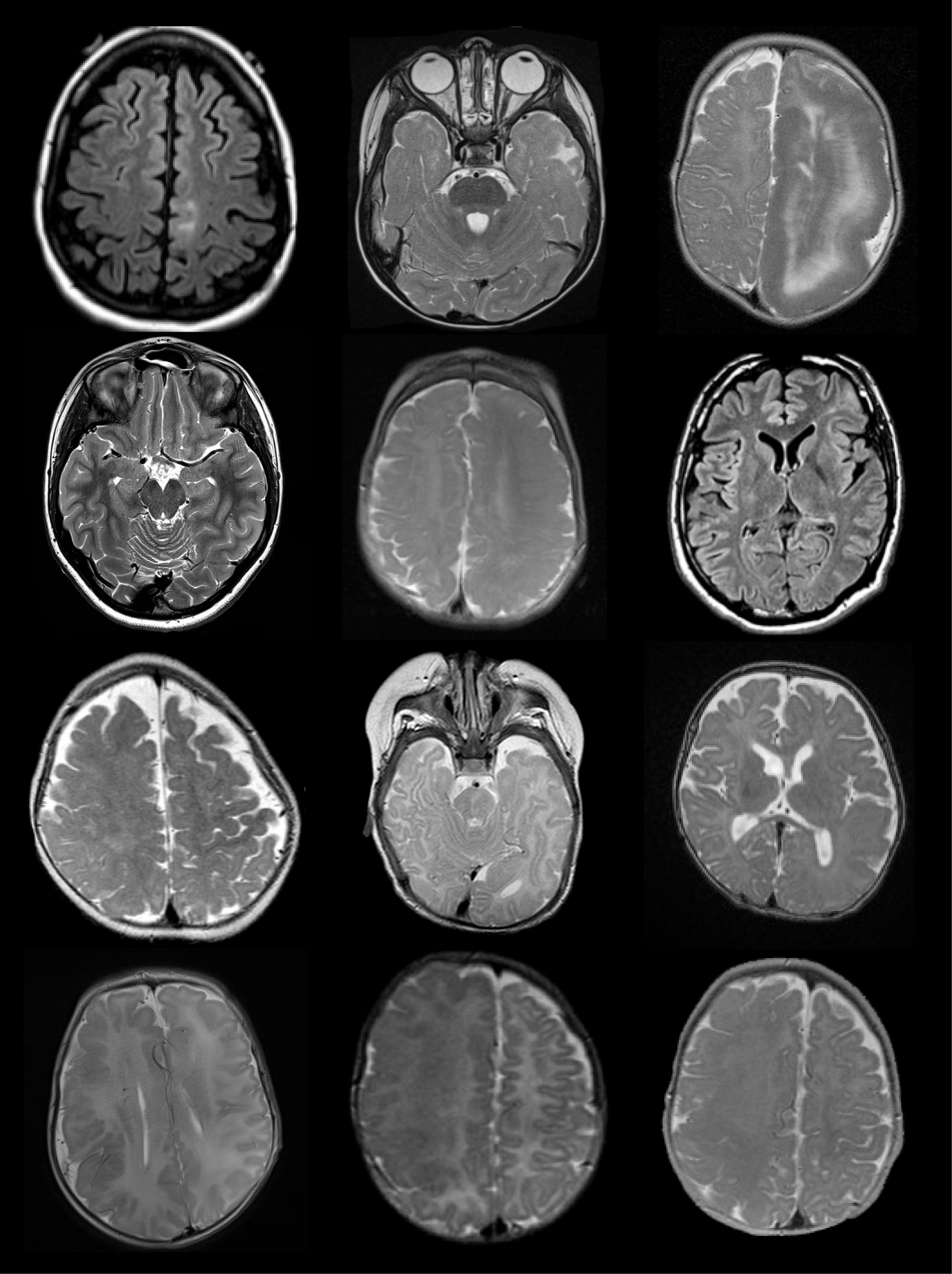
Mosaic (post-zygotic) variants that arise during fetal development and postnatal life are increasingly recognized to play an important role in neurological disorders. Previous work, including Dr. D’Gama’s graduate work, demonstrated that pathogenic mosaic variants in the mTOR pathway cause focal epilepsies associated with malformations of cortical development (Focal Cortical Dysplasia Type II and Hemimegalencephaly). However, the true contribution of somatic mosaicism to epilepsy is unknown. We discover brain-limited and non-brain limited mosaic variants underlying pediatric epilepsies using deep sequencing, optimized bioinformatics analyses, and validation. We are also interested in developing new diagnostic methods to detect mosaic variants in patients with epilepsy and implementing genetic testing for mosaic variants into clinical epilepsy care.
fetal and neonatal neurogenetics
Many neurological conditions present during the fetal and neonatal periods, including brain malformations, seizures, hydrocephalus, hypoxic-ischemic injury, stroke, intraventricular hemorrhage, periventricular leukomalacia, infections affecting the brain, hypotonia, and neural tube defects. Infants with these conditions often require specialized care after birth in the Neonatal Intensive Care Unit. We are interested in understanding how genetic factors may cause these conditions or interact with environmental factors to contribute to these conditions.
NEONATAL GENOMICS
Many infants admitted to Neonatal Intensive Care Units (NICUs) have known or suspected genetic disorders. We are interested in discovering genetic diagnoses for these infants, optimizing the use of genetic testing in NICU settings, and equitably expanding access to genetic testing, especially rapid sequencing, in NICU settings.